Stening® Thin Wall Tracheal Stent
Code HE

Description
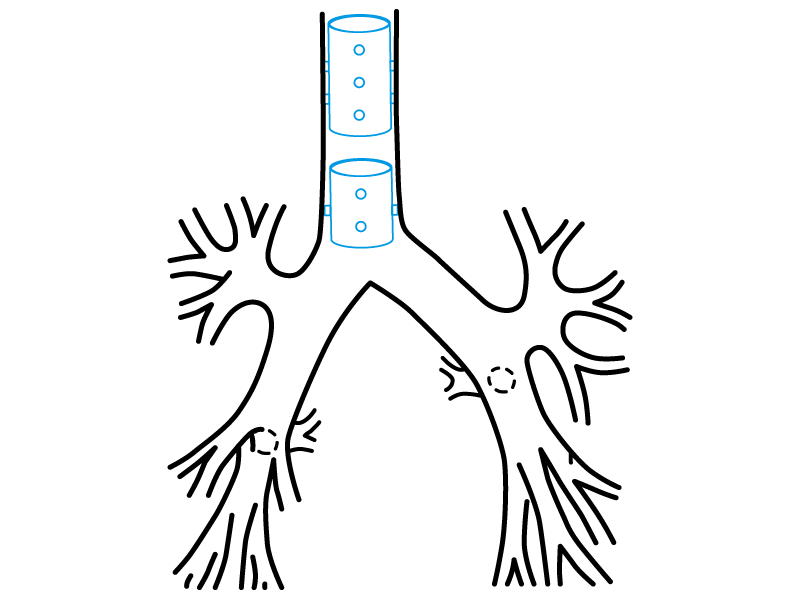
It consists on a straight tracheal stent with a thinner wall. This docility makes its implant and removal easier.
It has a special utility after the neoplastic and endotracheal tissue’s resection, when the affection lacks of a compressive component.
Distinctive features:
A thinner wall of the prosthesis significances an increase in the stent cross section surface destined for ventilation.
The relation between the surface that occupies the wall and the clearance available for ventilation is modified favourably.
In the other way round, it can be expected a lower resistance to extrinsic compression and a decrease of the cession point.
The wall’s thickness decrease makes easier the introduction of the prosthesis inside the ejector or the bronchoscope. As well as the implant and removal manoeuvres.
Stening® provides detailed instructions for each device, including insertion and removal techniques, precautions and postoperative cares.
- Stening ST with 1.5 mm thickness (with a somewhat higher radial pressure).
- Stening SAP with 2 mm thickness (more robust wall, with high radial pressure)
- Primary or secondary tracheal neoplasm
- Tracheoesophageal fistula
- Tracheal rupture
- After laser resection, cryotherapy or electrocautery, to maintain the airway opened
- Tracheomalacia
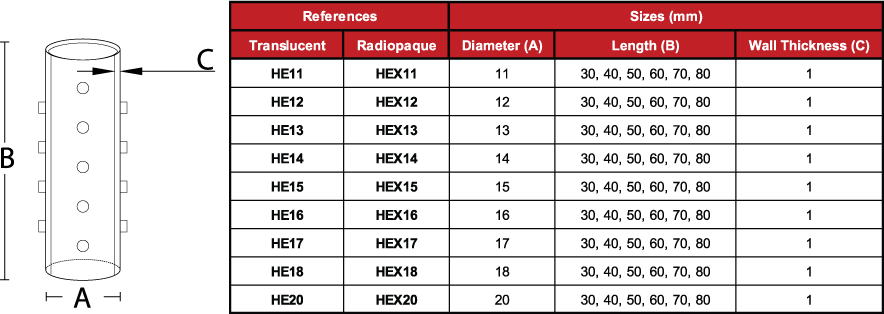
Due to the characteristics of the production process, the
measurements of the devices can vary by +/- 2%
- Medical grade silicone
- Bevelled edges to prevent granulomas
- Spur system to prevent migration
- Removable
- Surface of maximum softness to avoid adherence of secretions
- Transparent or Radiopaque
Introduction technique:
The procedure will take place under general anaesthesia.
The implant of these type of prostheses can be made directly through the work channel of the tracheoscope or bronchoscope.
A conventional introducer for silicone prostheses can be used as well. A rigid endoscope will be used to access the airway.
The length and diameter of the area that the stent will cover must be established correctly.
If you want to know the length of the area, you can mark the tracheoscope when its extreme is located at the end of the injury. Repeat the process once the tracheoscope is moved up to the beginning of the injury. The diameter of the trachea or bronchi must be estimated by comparing it with the diameter of the endoscope used.
Retrograde mode of Implant:
- Lubricate the introducer nozzle with lidocaine gel, preventing the lubricant from reaching the operator’s fingers.
- Fold the Stening® over its axial axis and put it inside the prostheses introducer through its nozzle.
- Remove the nozzle.
- Surpass the injured area with the tube of the tracheoscope and put its distal edge over the healthy mucosa, exceeding from 5 to 7 mm the affected zone.
- Put the introducer inside the tracheoscope.
- Press the ejector while the tracheoscope is removed and the ejector plunger progresses. That is, the plunger of the stents’ charger has to be pressed as the endoscope is removed.
In this way, the prosthesis will be released. If it is necessary, it can be moved to a better position with an alligator forceps. The manoeuvre is much easier when the stent is lower than the injury.
Antegrade mode of implant:
Steps 1 to 3 will be repeated.
You have to stop the tracheoscope that contains the introducer and the prosthesis 5 mm before the injury.
After that, you have to press the ejector plunger slowly. By doing this, the prosthesis will be expelled into the injured trachea.
Some stents’ charger models are not introduced inside the tracheoscope, but they are added to the proximal extreme, from where the stent is expelled. To accomplish this, the endoscope will have to be stopped in a proximal or distal way to the injury, as it was explained before, to push the prosthesis with the plunger that is provided with the endoscopic instrumental. In this way, the stent will travel through the tracheoscope until it reaches the trachea. At this point, we will feel a small reduction of the resistance in the pressure performed on the plunger, showing that the stent has begun to abandon the endoscope interior.
Correction of the stent position:
The stent may require some additional manoeuvres, focusing on correcting or adjusting its final position.
It is preferable to correct stent that has been installed beyond the desired position than the opposite, due to the arduousness of pushing a stent that has been released before the damaged zone.
To move a stent in a proximal way, it can be taken by its edge and then you must pull with kindness.
To be more accurate we recommend a manoeuvre that consists on taking the stent by its edge as it was mentioned before. After that, you have to advance with the optical vision through the stent’s inside until you see its ending. Now pull the forceps and you will be able to see how the stent ascends through the airway.
Stop the pulling as long as you consider that the position is correct.
Extraction technique:
We will proceed to the intubation with the tracheoscope or the rigid bronchoscope depending on the case.
Of easy extraction, the silicone stent must be taken by its proximal edge with a crocodile forceps, with enough steadiness. Rotate the forceps 360º so that the stent bends, acquiring an omega shape and losing its radial resistance to compression. Then, pull the forceps and extract the prosthesis together with the tracheoscope.
The stent proximal edge can be introduced inside the tracheoscope. With this manoeuvre the vocal chords are protected during the extraction.
Other implant and removal methods are also possible depending on the experiences and preferences of the surgeon.
- Maintain the moisture of secretions, whenever they appear, by taking nebulisations frequently with a warm isotonic saline solution.
- Perform a periodic check-up following your doctor’s advice.
- Take care of your oral hygiene and treat cavities.
The product should not be reused because this can cause cross contamination.
A sterile non-bioabsorbable tubular device intended to be implanted into the trachea and/or a bronchus/bronchiole to maintain luminal patency, typically used in cases of obstructions/stenoses, fistulae, tumours, scarring, surgical resection and anastomosis, or pulmonary transplantation. It is made entirely of a synthetic polymer(s) [e.g., silicone] and may have various designs (e.g., semi-soft continuous tube, covered or non-covered mesh structure, straight or branched configuration) intended to conform to the endotracheal/endobronchial surface. It may be expandable in situ (e.g., self-expands) and disposable devices intended to assist implantation may be included.
46977